2.1 What happened at Lake Alice Ngā āhuatanga i hua ake i Lake Alice
WARNING: DISTRESSING CONTENT
2.1.1 Te whakatūnga o te manga tamariki me te rangatahi ki Lake Alice - Establishment of the Lake Alice child and adolescent unit
46. Lake Alice Hospital was built in 1950 as a regional psychiatric centre. As with other psychiatric hospitals built in Aotearoa New Zealand in this era, the design of the hospital reflected changing ideas about mental illness and its treatment. The design rejected the older asylum model of imposing single buildings, by housing patients in a series of ‘villas’. As well as aiming to create a more ‘home-like’ environment for patients, the villa system allowed for the greater separation of patients by age, gender, behaviour or perceived likelihood of recovery.[80]
47. The hospital was designed to be, as far as possible, a self-sufficient township. Services such as a laundry, butchery, bakery, library and garage were all on site, and staff lived in accommodation on hospital grounds.[81] The farm and large vegetable gardens on the land were intended to provide meat, dairy and fresh produce for the hospital, making it largely self-supporting, as well as providing ‘useful’ labour for hospital patients.[82]
48. Lake Alice had a multidisciplinary workforce consisting of psychologists, psychiatrists, medical officers, nursing staff, occupational therapists, pharmacists, physiotherapists, recreation officers, dentists and, later, teachers.[83] These were supported by a range of staff who ran the hospital, including cooks and grounds people, many of whom were locals from around Marton. Some were mana whenua from Ngā Wairiki and Ngāti Apa.
49. Most of the hospital’s medical and nursing staff lived with their families in housing on the hospital grounds or in houses bought by the hospital in nearby Marton. By 1972, there were at least 40 houses on the grounds and 16 more
in Marton.[84]
50. In July 1970, the hospital’s medical superintendent, Dr Sydney Pugmire, acknowledged the hospital had “no special facilities for children” and avoided admitting them “as far as possible”. However, 11 children had been admitted and treated that year.[85] Lake Alice’s annual reports show in 1970[86] and 1971,[87] over the two years before the opening of the Lake Alice child and adolescent unit, 34 children and 59 youths spent some time at the hospital.
51. Dr Selwyn Leeks started seeing young patients at Lake Alice from as early as June 1971.[88] At this time, there was no designated child and adolescent unit so young patients were housed in general villas. From 9 November 1971, Dr Leeks accepted responsibility as psychiatric consultant for all patients at Lake Alice under the age of 17.[89] He also worked at two other child health clinics, one in Whanganui and another at Palmerston North Hospital.[90]
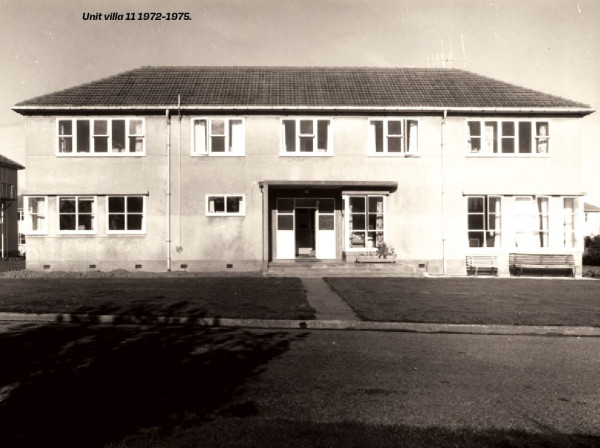

52. In August 1972, the hospital set up a dedicated unit in an existing building for children and adolescents. This was initially a 12-bed villa for boys,[91] which was known as villa 10.[92] The unit’s capacity grew quickly. A second 12-bed villa for boys was added later in 1972,[93] which was known as villa 11.[94]
53. In October 1972, Dr Pugmire told the Department of Health’s Director of Mental Health, Dr Stanley Mirams, the hospital had set up a wing for adolescents, separating them from the adult wards, because “we have admitted a hundred extremely difficult children during the past year, some of whom have engaged in calculated and well-planned attacks on both patients and staff”.[95] He mentioned one incident that left a nurse with injuries, including a broken nose.[96] He went on, “To keep this violent group separate from our well-behaved, respectable mentally ill new admissions, we have opened a separate teenage training villa and we are trying to develop an incentive training programme”.[97]
54. Although the unit’s dedicated villas housed only boys, Dr Leeks also treated girls at Lake Alice. Girls were initially housed in the adult admission villa, which accommodated both men and women, but spent their days in the unit.[98] Later, eight to 10 girls were accommodated in one wing of the women’s villa.[99] Eventually, the two boys’ villas proved insufficient, and the boys were transferred to a larger, 36-bed villa on 27 June 1975 (villa 7). It was filled throughout 1975.[100]
55. Charge nurse, Dempsey Corkran, told us he had concerns about adult patients having sex with children and young people at the unit. He said this was the reason he wanted the boys moved to villa 7, so they would be accommodated separately from the admissions ward, which housed adult patients.[101] Villa 7 was self-contained, so children and young people at the unit did not need to share facilities with patients from other villas.

56. Nursing staff organised some school classes when the unit opened,[102] but as more children and young people were admitted for extended periods of treatment, the Department of Education acknowledged the “possible” need for a teacher to ensure continuity of education.[103] A school was established at the hospital in February 1973.[104] The government recognised continued education for most young patients at Lake Alice school was an “important part of the whole treatment programme...”[105] The Department of Education summarised the aims of the school:
“[I]n ascending order, the aims are to have the child return to his school – educationally no worse off for his period in the Hospital; having had the benefit of more individualised teaching; performing at a considerably better level than previously.” [106]
57. The number of staff associated with the Lake Alice school expanded over time as the school roll grew. By 1974, the school had a full-time play therapist on staff, in addition to two full-time teachers.[107] The school was administered by the Whanganui Education Board, which was responsible for the provision of teaching staff, furniture and equipment. The Department of Health was responsible for the provision and maintenance of suitable accommodation. A former principal of the school noted the difficulties in the school being managed by different institutions:
“All this oversight made it a complicated system and every time we wanted to do something or improve something, everybody would just disappear, especially if they thought there was any blame involved. Furthermore, if anything worthwhile happened, everybody would jump up and down and say ‘yes, that was our idea’[108] … getting anything from the Educational Board in the way of money for teacher aid or anything of that nature was like drawing hens’ teeth”.[109]
58. The rapid growth in students was understood by the Department of Education as an administrative issue.[110] Throughout the years, the roll shifted from 19 students in 1973 (with 60 students attending throughout various periods) to 43 students in 1976 and then dropped to 32 students in 1977.[111]
59. An assessment of the school’s performance in 1977 found the school to be on the lowest level, the “maintenance level”, which meant the school was preventing students’ further educational decline during their period of hospitalisation.[112] The 1977 report said, due to staffing issues, it was unlikely students would be able to make “normal progress in their studies”.[113] At that time, the staff were made up of four primary teachers, who couldn’t always provide the support needed by secondary school students in the unit.[114] The report continued:
“This is indeed unfortunate for, as a result of the conditions which bring [the students] to Lake Alice, they are usually already under achievers upon arrival. If, while patients, their educational retardation is increased their chances of being rehabilitated in the schools from which they come are markedly reduced.”[115]
60. This report foretold what many survivors said happened to them: their education was badly affected by their admission to Lake Alice. We discuss this further in chapter 2.2.
Dr Leeks
Selwyn Robert Leeks was born in 1929.[116] Between 1953 and 1960, he completed bachelors degrees in science, medicine and surgery at the University of New Zealand.[117] From 1959, he worked at various medical, psychiatric and educational jobs in New Zealand and England.[118] In 1969, he received a diploma of psychological medicine from the Royal College of Physicians and Surgeons in London, and in 1971, he received a diploma in child psychiatry from the University of Otago.[119]
In February 1971, the Palmerston North Hospital Board hired Dr Leeks as a consultant child psychiatrist, and he held this position until he left New Zealand in 1977. [120] At the time, Dr Leeks was one of the few qualified child psychiatrists in New Zealand. He was the head psychiatrist in charge of the child and adolescent unit at Lake Alice Hospital from when it opened. Between 1973 and 1975, Ms Priscilla Leeks, Dr Leeks’ first wife, also worked at the unit as a child therapist.[121]
Although Dr Leeks lived in a house on hospital grounds, he only ever worked at the hospital part time.[122] He had a wide variety of duties in addition to psychiatry, including developing child health clinics, regularly visiting Kimberley Hospital and State residences Kohitere Boys’ Training Centre and Hokio Beach School, writing psychiatric reports on remand prisoners for courts, assessing armed forces personnel at bases in Waiouru, Linton and Ohakea, and lecturing and supervising psychology students at Massey University.[123]
Dr Leeks usually visited the unit only once a week, although sometimes he visited more frequently.[124]

